Endometriosis – an introduction
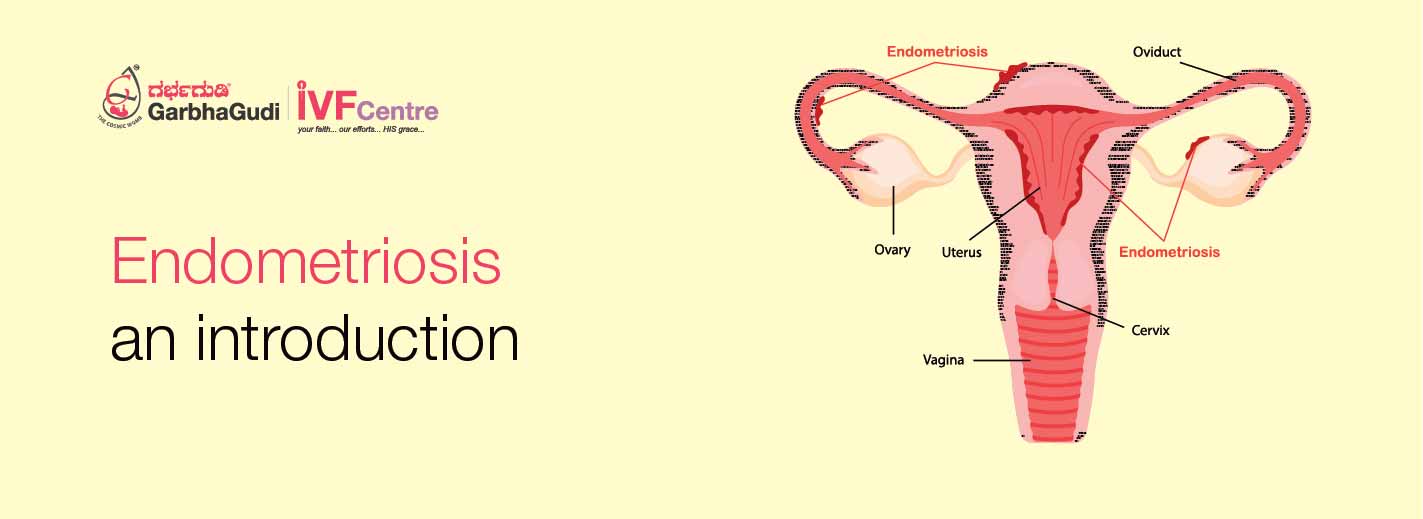
Endometriosis is an often painful disorder in which tissue that normally lines the inside of your uterus – the endometrium grows outside your uterus. Endometriosis most commonly involves your ovaries, fallopian tubes and the tissue lining your pelvis. Rarely, endometrial tissue may spread beyond pelvic organs. With endometriosis, displaced endometrial tissue continues to act as it normally would, it thickens, breaks down and bleeds with each menstrual cycle. Because this displaced tissue has no way to exit your body, it becomes trapped. When endometriosis involves the ovaries, cysts called endometriomas may form. Surrounding tissue can become irritated, eventually developing scar tissue and adhesions and abnormal bands of fibrous tissue that can cause pelvic tissues and organs to stick to each other. Causes Although the exact cause of endometriosis is not certain, possible explanations include:
Retrograde menstruation: Menstrual blood containing endometrial cells flows back through the fallopian tubes, into the pelvic cavity instead of out of the body. These displaced endometrial cells stick to the pelvic walls & surfaces of pelvic organs, where they grow and continue to thicken and bleed over the course of each menstrual cycle.
Transformation of peritoneal cells. In what’s known as the “induction theory,” experts propose that hormones or immune factors promote the transformation of peritoneal cells that line the inner side of your abdomen into endometrial cells.
Embryonic cell transformation. Hormones such as estrogen may transform embryonic cells — cells in the earliest stages of development into endometrial cell implants during puberty.
Surgical scar implantation. After a surgery, such as a hysterectomy or C-section, endometrial cells may attach to a surgical incision.
Endometrial cells transport. The blood vessels or tissue fluid (lymphatic) system may transport endometrial cells to other parts of the body.
Immune system disorder. It’s possible that a problem with the immune system may make the body unable to recognize and destroy endometrial tissue that’s growing outside the uterus.
Risk factors: Several factors place you at greater risk of developing endometriosis, such as:
> Never giving birth
> Starting your period at an early age
> Going through menopause at an older age
> Short menstrual cycles — for instance, less than 27 days
> Having higher levels of estrogen in your body or greater lifetime exposure to estrogen your body produces
> Low body mass index
> Alcohol consumption
> One or more relatives (mother, aunt or sister) with endometriosis
> Medical conditions that prevent the normal passage of menstrual flow out of the body
> Uterine abnormalities
Endometriosis usually develops several years after the onset of menstruation (menarche). Signs and symptoms of endometriosis end temporarily with pregnancy and end permanently with menopause unless you’re taking estrogen. Symptoms The primary symptom of endometriosis is pelvic pain, often associated with your menstrual period. Although many women experience cramping during their menstrual periods, women with endometriosis typically describe menstrual pain that is far worse than usual. They also tend to report that the pain increases over time. Common signs and symptoms of endometriosis may include:
> Painful periods (dysmenorrhea). Pelvic pain and cramping may begin before your period and extend several days into your period. You may also have lower back and abdominal pain.
> Pain with intercourse. Pain during or after sex is common with endometriosis.
> Pain with bowel movements or urination. You’re most likely to experience these symptoms during your period.
> Excessive bleeding. You may experience occasional heavy periods (menorrhagia) or bleeding between periods (menometrorrhagia).
> Infertility. Endometriosis is first diagnosed in some women who are seeking treatment for infertility.
> Other symptoms. You may also experience fatigue, diarrhoea, constipation, bloating or nausea, especially during menstrual periods.
> The severity of your pain isn’t necessarily a reliable indicator of the extent of the condition.
> Some women with mild endometriosis have intense pain, while others with advanced endometriosis may have little pain or even no pain at all.
> Endometriosis is sometimes mistaken for other conditions that can cause pelvic pain, such as pelvic inflammatory disease (PID) or ovarian cysts.
When to see a doctor
See your doctor if you have signs and symptoms that may indicate endometriosis. Endometriosis can be a challenging condition to manage. An early diagnosis, a multidisciplinary medical team and an understanding of your diagnosis may result in better management of your symptoms. When to get help when period pain is stopping normal daily activities. For example:
> missing work, school or recreational activities
> when medicines used for period pain don’t help reduce the pain
> when you need to stay in bed due to pain
> when symptoms are getting worse
> when you feel upset by your symptoms
> when your ability to cope mentally decreases