What Are the Layers of Endometrium? A Detailed Overview
What is the endometrium?
The endometrium is the innermost layer of the uterus, forming its lining. This vital tissue undergoes dynamic changes throughout the menstrual cycle in response to hormonal fluctuations. The endometrium is crucial for reproductive processes, particularly in facilitating embryo implantation and supporting a potential pregnancy.
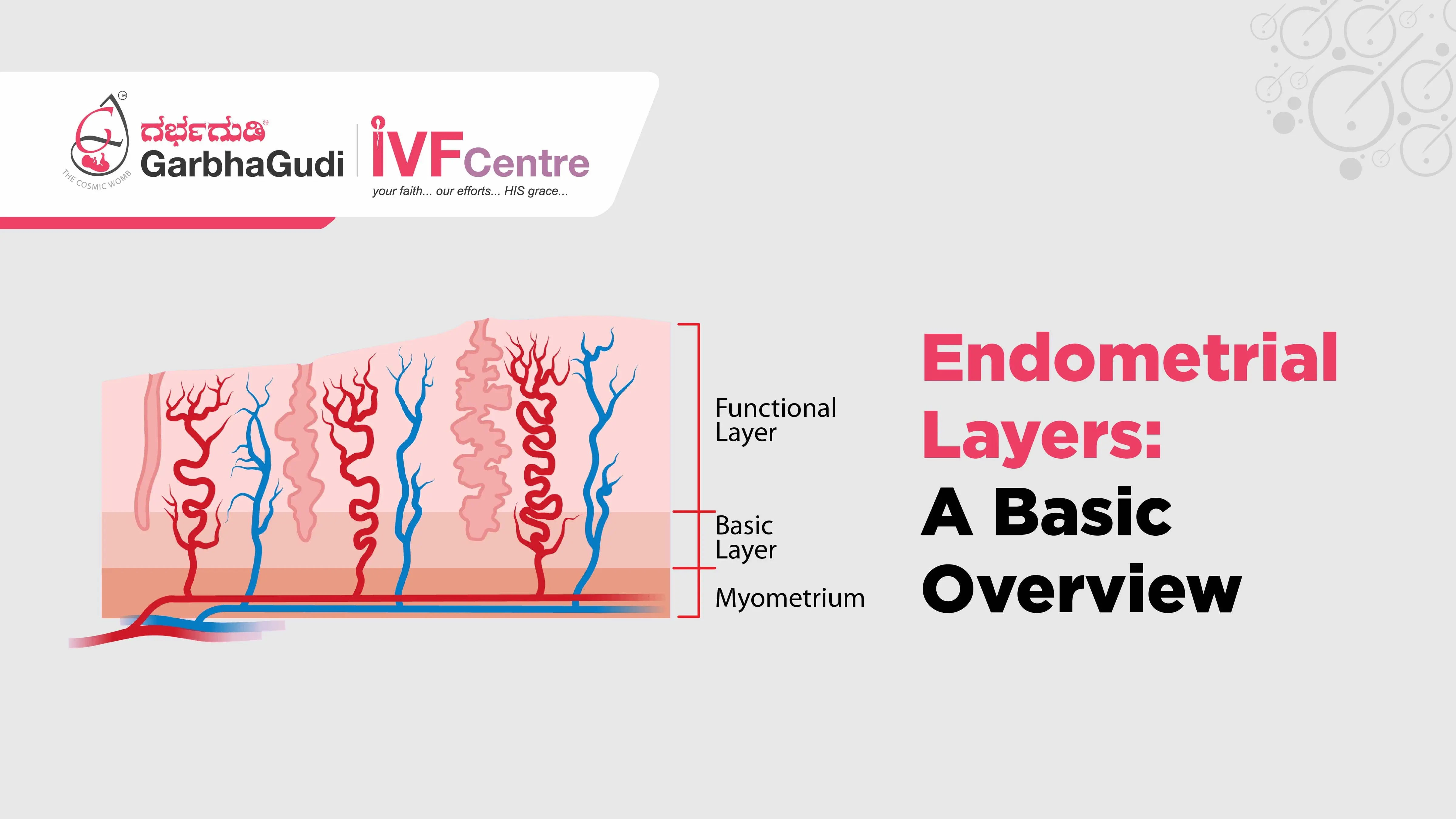
Basal Layer: The deepest layer remains relatively constant and serves as the foundation for endometrial regeneration.
Functional Layer: The middle layer experiences cyclic changes in response to hormonal signals during the menstrual cycle. If pregnancy does not occur, this layer is shed during menstruation.
Zona Compacta (Perimetrium): The outermost layer, also known as the perimetrium, covers the surface of the uterus.
The cyclical changes in the endometrium involve thickening and vascularization during the proliferative phase, preparing for potential implantation. If fertilization does not occur, the functional layer is shed, marking the beginning of the menstrual phase. Understanding the dynamics of the endometrium is crucial for assessing reproductive health, fertility, and conditions affecting the uterus.
What are the layers of the endometrium?
The endometrium, the innermost lining of the uterus, is a complex and dynamic tissue composed of three distinct layers, each playing a vital role in the menstrual cycle and reproductive processes.
Basal Layer:
The basal layer serves as the foundational component of the endometrium. It remains relatively constant throughout the menstrual cycle and acts as a source for regenerating the other layers. This layer plays a crucial role in providing structural support and facilitating the renewal of the functional layer.
Functional Layer:
The functional layer is the middle and most dynamic portion of the endometrium. It undergoes cyclical changes in response to hormonal fluctuations during the menstrual cycle. During the proliferative phase, stimulated by rising estrogen levels, this layer thickens and becomes more vascularized in preparation for potential embryo implantation. If fertilization does not occur, hormonal signals trigger the shedding of the functional layer during menstruation, marking the beginning of a new cycle.
Zona Compacta (Perimetrium):
The outermost layer of the endometrium is also referred to as the perimetrium or zona compacta. This layer covers the surface of the uterus, providing a protective and supportive structure for the entire endometrial lining.
The cyclic changes in the endometrium are intricately linked to the menstrual cycle and are crucial for the establishment and maintenance of a healthy pregnancy. Understanding these layers is essential in the context of reproductive health, fertility assessments, and addressing conditions that may affect the uterus. The ability of the endometrium to undergo these dynamic changes is fundamental to the success of reproductive processes, including embryo implantation and the progression of pregnancy.
What conditions can affect the endometrial layers?
Several conditions and factors can impact the health and structure of the endometrial layers, potentially affecting reproductive health and fertility. Some notable conditions include:
Endometrial Hyperplasia:
Abnormal thickening of the endometrium is often associated with an excess of estrogen without the counterbalance of progesterone. It can lead to irregular menstrual cycles and may increase the risk of developing endometrial cancer.
Endometriosis:
A condition where endometrial tissue grows outside the uterus, causing inflammation, pain, and the formation of adhesions. Endometriosis can affect the normal function of the endometrium.
Polyps:
Growth of abnormal tissue within the endometrial cavity. While often benign, polyps can impact fertility and may cause irregular bleeding.
Uterine Fibroids:
Noncancerous growths in the uterus that can distort the uterine cavity, potentially affecting the endometrial lining and fertility.
Asherman's Syndrome:
Formation of scar tissue (adhesions) within the uterine cavity, often due to surgical procedures. Asherman's Syndrome can lead to a reduction in the thickness of the endometrium and fertility challenges.
Endometrial Cancer:
Uncontrolled growth of cells in the endometrium, which can affect the normal structure and function of the endometrial layers. It is more common in postmenopausal women.
Hormonal Imbalances:
Conditions leading to imbalances in estrogen and progesterone levels can impact the cyclic changes of the endometrium, affecting its thickness and receptivity.
Age-Related Changes:
Natural aging processes can influence the endometrial layers. In postmenopausal women, there is a decline in estrogen levels, leading to thinning of the endometrial lining.
Infections or Inflammation:
Infections or inflammatory conditions of the uterus can disrupt the normal architecture of the endometrial layers.
Latrogenic Causes:
Surgical procedures, particularly those involving the uterus (e.g., dilation and curettage - D&C), can sometimes result in scarring or damage to the endometrial lining.
Understanding and addressing these conditions are crucial for maintaining the health of the endometrial layers and ensuring optimal reproductive outcomes. Individuals experiencing irregular menstrual cycles, abnormal bleeding, or fertility concerns should seek medical evaluation for a thorough assessment and appropriate management.
What are the common symptoms of endometrial issues?
Endometrial issues can manifest with various symptoms, and the severity and nature of these symptoms can vary depending on the specific condition affecting the endometrium. Common symptoms of endometrial issues include:
Abnormal Uterine Bleeding:
Irregular menstrual cycles.
Heavy or prolonged menstrual bleeding.
Spotting between periods.
Pelvic Pain:
Chronic pelvic pain, which may be dull or sharp.
Painful menstruation (dysmenorrhea).
Pain during or after sexual intercourse (dyspareunia).
Changes in Menstrual Patterns:
Changes in the length or regularity of menstrual cycles.
Absence of menstruation (amenorrhea) or infrequent periods.
Painful Menstruation:
Severe menstrual cramps that interfere with daily activities.
Infertility:
Difficulty conceiving or recurrent pregnancy loss.
Painful or Frequent Urination:
Endometriosis or uterine fibroids pressing on the bladder may cause pain or increased urgency to urinate.
Back Pain:
Pain in the lower back, often associated with menstruation.
Bloating or Swelling:
Abdominal bloating or a feeling of fullness, especially with conditions like endometriosis.
Unintended Weight Loss or Gain:
Changes in weight that are not attributed to intentional efforts.
Fatigue:
Persistent fatigue or low energy levels.
Gastrointestinal Symptoms:
Digestive issues such as constipation or diarrhea, especially with conditions like endometriosis.
Symptoms Postmenopause:
Vaginal bleeding or spotting after menopause is a concerning symptom that should be promptly evaluated.
It's important to note that these symptoms may not solely indicate endometrial issues and can be associated with various gynecological conditions. If individuals experience persistent or severe symptoms, seeking medical attention is crucial for a comprehensive evaluation, accurate diagnosis, and appropriate management. Timely intervention can help address underlying issues and improve reproductive and overall health.
What is the significance of a thickened or thin endometrium?
The thickness of the endometrium holds significance in the context of reproductive health and fertility, and it is often assessed during various stages of the menstrual cycle and fertility treatments. Both a thickened and a thin endometrium can have implications, and their significance depends on the specific circumstances:
Thickened Endometrium:
Significance:
During the proliferative phase of the menstrual cycle, a thickened endometrium is generally considered favorable for potential embryo implantation.
In the context of fertility treatments like in vitro fertilization (IVF), an adequately thick endometrium is desired for optimal chances of successful embryo implantation.
Possible Causes:
Adequate hormonal support, particularly estrogen, contributes to endometrial thickening during the proliferative phase.
Conditions like endometrial hyperplasia, polyps, or hormonal imbalances may also lead to a thickened endometrium.
Clinical Implications:
A thickened endometrium may be advantageous for achieving and maintaining a healthy pregnancy, but extreme thickness may warrant further investigation.
Thin Endometrium:
Significance:
A thin endometrium may pose challenges for successful embryo implantation and may be associated with reduced fertility.
In fertility treatments, particularly IVF, a thin endometrium may be a concern, impacting the chances of successful implantation.
Possible Causes:
Insufficient hormonal support, particularly estrogen, may result in a thin endometrium.
Age-related changes, hormonal imbalances, or conditions like Asherman's syndrome (uterine adhesions) can contribute to endometrial thinning.
Clinical Implications:
Addressing the underlying causes of a thin endometrium is essential, and interventions may be needed to optimize endometrial thickness for successful conception.
While endometrial thickness is a crucial factor, it's important to note that other factors, including endometrial receptivity and overall uterine health, also influence reproductive outcomes. A comprehensive assessment by healthcare providers is necessary to understand the specific context and address any concerns related to endometrial thickness in the context of fertility and reproductive health.
How does the endometrial lining impact fertility treatments?
The endometrial lining plays a crucial role in the success of fertility treatments, especially those involving assisted reproductive technologies. Here's how the endometrial lining influences fertility treatments:
Optimal Environment for Implantation:
A thick and receptive endometrial lining is essential for the successful implantation of an embryo. The lining provides the necessary support and nourishment for the developing embryo.
In Vitro Fertilization (IVF):
In IVF, the embryo is cultured in a laboratory setting before being transferred into the uterus. A well-prepared endometrial lining is crucial for the embryo to implant successfully.
Embryo Transfer:
The thickness and quality of the endometrial lining are assessed before embryo transfer in IVF. An ideal lining provides a favorable environment for the embryo to attach to the uterine wall.
Timing of Procedures:
Fertility treatments are often timed in alignment with the natural menstrual cycle. Monitoring the endometrial thickness helps ensure that the uterus is in an optimal state for embryo implantation.
Hormonal Support:
Hormonal medications are often used in fertility treatments to regulate the menstrual cycle and support the development of the endometrial lining. Estrogen is commonly administered to enhance endometrial thickness.
Addressing Thin Lining Issues:
In cases where the endometrial lining is thin, additional interventions may be considered. This can include adjustments to medication protocols, the use of supplemental therapies, or exploring underlying factors that may be affecting the lining.
Frozen Embryo Transfer (FET):
In FET cycles, embryos are frozen and stored for later transfer. The timing of the embryo transfer is coordinated with the development of a receptive endometrial lining, increasing the chances of a successful implantation.
Monitoring During Treatment:
Throughout fertility treatments, ultrasound examinations are commonly used to monitor the thickness and appearance of the endometrial lining. This information guides healthcare providers in optimizing the conditions for successful implantation.
Impact on Pregnancy Rates:
Research suggests that an adequately thick endometrial lining is associated with higher pregnancy rates in fertility treatments. However, other factors, including endometrial receptivity, also play a role.
Addressing any issues with the endometrial lining, whether it's thinning or other abnormalities, is an integral part of fertility care. Individualized treatment plans are designed to optimize the conditions for successful embryo implantation and increase the likelihood of a healthy pregnancy.
The endometrial lining holds a pivotal role in the success of fertility treatments, particularly those involving assisted reproductive technologies. Its optimal thickness and receptivity are crucial factors influencing the likelihood of successful embryo implantation and, subsequently, a healthy pregnancy.
Throughout fertility treatments like In Vitro Fertilization (IVF) and embryo transfer, healthcare providers carefully monitor the endometrial lining. An adequately thick and receptive lining provides a favorable environment for the embryo to attach to the uterine wall, supporting its growth and development.
Hormonal support, precise timing of procedures, and interventions to address issues such as thin endometrial lining are integral components of fertility care. The use of medications, supplemental therapies, and adjustments to treatment protocols are tailored to each individual's unique needs, aiming to optimize the conditions for successful conception.
The close monitoring of the endometrial lining during fertility treatments underscores its significance in the overall reproductive process. Research suggests a positive correlation between an optimally thick endometrial lining and higher pregnancy rates. However, the interplay of various factors, including endometrial receptivity, emphasizes the need for a comprehensive and personalized approach to fertility care.
As individuals and healthcare providers collaborate on the fertility journey, attention to the health and condition of the endometrial lining remains central. By addressing any issues and ensuring an optimal environment for embryo implantation, fertility treatments aim to increase the chances of achieving the desired outcome—a healthy and successful pregnancy.